Granular Dystrophy Status Post Bilateral Keratectomy: John Koehler, OD, FAAO, FSLS
Background
A 67-year-old Caucasian female with bilateral granular dystrophy presented to have her habitual gas permeable (GP) lenses refit in both eyes. She had been an GP wearer for several decades. The patient stated that she felt her vision was worsening at both distance and near. She reported wearing the lenses twelve to fifteen hours per day, denied sleeping in the lenses, and used Boston Simplus solution to clean and store the lenses. She reported that her lenses would frequently get dirt and debris under the lenses when she was in remote environments working with Doctors Without Borders as a nurse and that with her current monovision correction she had a hard time seeing things at near unless they were held very close. She was not taking any medications and was using Refresh artificial tears for relief of dry eyes when wearing the lenses. This case demonstrates the use of scleral lenses to correct corneal irregularity in a patient with advanced Type I Granular Dystrophy status post repeat bilateral keratectomy procedures.
Test Procedures, Fitting/Refitting, Design, and Ordering
Visit #1: Initial Visit
Unaided Distance Visual Acuities
OD: 20/400 (Pinhole 20/150)
OS: 20/400 (Pinhole 20/100)
Visual Acuities with Monovision GPs
Distance acuity with both eyes open: 20/70
Near acuity with both eyes open: 20/100
Subjective Refraction
OD: +4.50 -2.25 x 162 (20/70+1)
OS: +2.50 -0.50 x 099 (20/50+2)
ADD: +3.00, 20/70 OD and 20/50 OS
Pupils were equal, round, and reactive to light; no afferent pupillary defect was noted. Confrontation fields were full to finger counting in both eyes. Extraocular motilities were smooth and full OU. Cover test was orthophoric at distance and four exophoric at near. Intraocular pressure with noncontact tonometry was 10 mmHg OD and 9 mmHg OS at 9:39 AM.
Anterior and Posterior Segment Examination
Anterior segment evaluation by slit lamp examination revealed no anomalies of the ocular adnexa, normal lashes and lid margins, and a quiet bulbar and palpebral conjunctiva. The cornea was remarkable for advanced, central, coalesced, granular hyaline deposits in both eyes, right more than the left. Tear break-up-time was five seconds in each eye. The anterior chamber was deep and quiet in each eye. The iris was flat, blue, and intact in both eyes. The lenses were clear. The patient was dilated with one drop of 1% phenylephrine and 2.5% tropicamide and findings were unremarkable in both eyes.
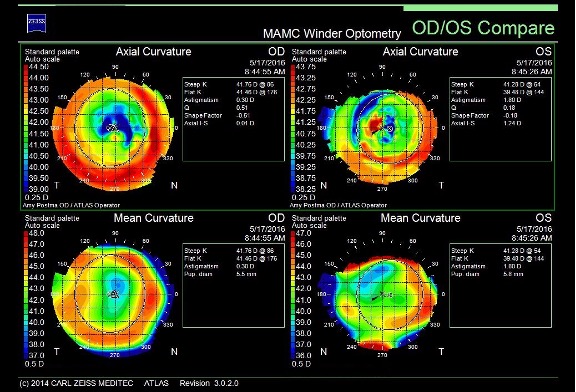
Corneal Topography
Corneal topography was remarkable for significantly irregular astigmatism in both eyes. Large hyaline deposits were visibly raising the epithelium to observation with thin beam on slit lamp examination that correlated to the raised areas on the ocular surface on the topography below. Due to the significant irregularity and the prior issues with discomfort with objects on or under the lens, a trial fitting of scleral contact lenses was initiated.
Scleral Lens Fitting
The patient was measured to have an HVID of 11.5 mm and a 16.8 mm diameter (Dia) Valley Custom Stable Elite (VCSE) lens set was selected. The VCSE lens has a standard central base curve (BC), with a midperipheral reverse curve, and a bitoric edge design with one meridian being six steps flatter than standard and another meridian 90 degrees away four steps steeper than standard. The value of a “step” is a proprietary measurement. They state that an adjustment to the scleral landing zone (SLZ) will alter the fit approximately 30 µm and a change to the limbal clearance zone (LCZ), approximately 100 µm per step change. The flat meridian of the edge is demarcated by having a laser etched oval on opposite sides of the lens. The steep meridian can then be found 90 degrees from the oval markings as shown in the drawing in Figure 2. Studies have shown that the scleral landing zone is either toric or irregular in most patients.
Initial Diagnostic Lenses
OD: VCSE, 7.85 BC, 16.8 Dia, std LCZ, std +6/-4 SLZ, -2.00 DS
OS: VCSE, 7.85 BC, 16.8 Dia, std LCZ, std +6/-4 SLZ, -2.00 DS
The lenses were applied on the eye and allowed to settle for twenty minutes. The lenses were evaluated via slit lamp examination (SLE), and central corneal clearance was approximately 330 µm OD and 380 µm OS estimated by comparing the central lens thickness to the vault. The lenses were judged to have slightly excessive central clearance and a move to a flatter base curve was made in both eyes.
Second Diagnostic Lenses
OD: VCSE, 8.23 BC, 16.8 Dia, Std LCZ, std +6/-4 SLZ, Pl Sph
OS: VCSE, 8.23 BC, 16.8 Dia, Std LCZ, std +6/-4 SLZ, Pl Sph
After 20 minutes the central corneal clearance was approximately 190 µm OD and 290 µm OS. The right lens was taken out and replaced with the former trial lens.
Final Diagnostic Lenses
OD: VCSE, 7.85 BC, 16.8 Dia, std LCZ, std +6/-4 SLZ, -2.00 DS
OS: VCSE, 8.23 BC, 16.8 Dia, Std LCZ, std +6/-4 SLZ, Pl DS
With SLE the central corneal clearance was approximately 300 µm OD after 20 minutes, and 260 µm OS after 40 minutes. The tear layer feathered out past the limbus 360 degrees in both eyes. No evidence of compression or impingement were observed in either eye, but both eyes demonstrated a slight edge lift at the flat meridian temporally. The flat SLZ meridian was noted to be at 45 degrees to the right and the left lens was noted to be 45 degrees to the left (see Figure 2). Both lenses rotated easily to light pressure and were well centered.

Over-Refraction (OR):
OD: +2.00 -0.50 x 041 (20/40)
OS: +2.25 -0.50 x 126 (20/30-1)
The patient preferred to stay in monovision correction. Sensory dominance was tested with a +1.00DS blur test, revealing that her OS was her sensory dominant eye. A +3.00D add over the right eye revealed a 20/30 near correction at 30 cm working distance.
Initial Lens Order: The flat meridian was ordered one step steeper from a +6/-4 to a +5/-4 OU.
OD: VCSE, 16.8 Dia, 7.85 BC, std LCZ, +5/-4 SLZ, +4.75 DS, Optimum Extra, blue (near)
OS: VCSE, 16.8 Dia, 8.23 BC, std LCZ, +5/-4 SLZ, +2.00 DS, Optimum Extra, clear (distance)
Patient Consultation and Education
Visit #2: Dispense Appointment
The patient reported for follow up approximately one month later and the lenses were evaluated after one hour of wear time.
Slit Lamp Evaluation
Central clearance was approximately 280 µm OD and 260 µm OS. The lenses had limbal clearance 360 degrees in both eyes, no evidence of compression or impingement were observed in either eye.
Visual Acuity
OD: 20/30+2 @ 20 cm (near) OR: -1.25 DS (20/30-1 @ 33 cm)
OS: 20/40+1 (distance) OR: +0.25 -0.25 x 010 (20/40)
The patient complained that the near eye was too strong and that she needed to hold things too close to see clearly, and requested a reorder of the OD lens with modified power.
Application, Removal, and Care Education
The patient completed application and removal training and the above lenses were dispensed until the reordered OD lens arrived. Cleaning with overnight hydrogen peroxide solutions and daily cleaning/mechanical rubbing with either Lobob Optimum or Boston Simplus solutions was recommended.
Follow-up Care and Final Outcome
Visit #3: 1 Month Follow-Up
The patient reported for follow up approximately one month later and reiterated her prior complaint of the near prescription being over corrected and that it was uncomfortable for her to hold her reading material so close.
Slit Lamp Evaluation
The patient had been wearing the lenses for approximately three hours. Central clearance was approximately 250 µm OD and 240 µm OS. The lenses had limbal clearance 360 degrees in both eyes, no evidence of compression or impingement were observed in either eye. Both lenses were removed and sodium fluorescein (NaFl) was used to evaluate for lens off stain, and no stain was present in either eye.
The left lens was reinserted and the right lens was replaced with the updated prescription:
OD: VCSE, 16.8 Dia, 7.85 BC, std LCZ, +5/-4 SLZ, +3.50 DS, Optimum Extra, blue (near)
OS: VCSE, 16.8 Dia, 8.23 BC, std LCZ, +5/-4 SLZ, +2.00 DS, Optimum Extra, clear (distance)
The patient was released from the clinic for three hours to allow lenses to settle and give the patient adequate time to test the updated power of lenses. Upon returning she reported much more comfortable vision and appropriate working distance with the lenses.
Visual Acuity
OD: 20/40 @ 33 cm (near) OR: Pl DS (20/40)
OS: 20/40 (distance) OR: +0.25 DS (20/40)
Application and removal techniques, lens hygiene, and wear time of 12-14 hours per day was reviewed with the patient. She was very happy with the outcome of improved vision and comfort in the lenses. The lenses were released and she was advised to return to the clinic every six months for progress checks.
Visit #4: Seven Month Follow-Up
The patient reported for follow up approximately seven months later. She reported that vision and comfort remained very good during lens wear. She reported that although her working distance for near was now clearer, she was having a hard time reading small medication labels for her job as part time nurse.
Slit Lamp Evaluation
The patient had been wearing the lenses for approximately four hours. Central clearance was approximately 250 µm OD and OS. The lenses had limbal clearance 360 degrees in both eyes, no evidence of compression or impingement were observed in either eye. Both lenses were removed and sodium fluorescein (NaFl) was used to evaluate for lens off stain, and no stain was present in either eye.
Visual Acuity
OD: 20/40-1 @ 33 cm (near) OR: Pl DS (20/40)
OS: 20/40+1 (distance) OR: +0.25 DS (20/40+2)
No change to the lens prescription was recommended and patient was advised to continue current lens hygiene regimen and wearing schedule. Due to the patient complaint of trouble with fine detail, near tasks were addressed with low vision devices. Once the irregularity of the corneas was corrected with the scleral lenses, magnification devices were utilized to enlarge images to be able to provide resolution around corneal opacities secondary to advanced dystrophy observed in figures 4 and 5 below.


The following two devices were trialed and demonstrated for the patient successfully:
1. Optelec 3.5x Hand Magnifier with LED light
2. Optelec Power Scope Extra Short Focus 5×20, 11 deg-distance viewing
Both devices were the lowest power devices in the clinic’s low vision trial set. The added magnification was accounted for with working distance demonstration. The Power Scope has adjustable focus and the Hand Magnifier still allowed the patient to work at appropriate working distances. Both devices were released to the patient and a three-month progress check was scheduled.
Visit #5: Three Month Follow-Up with Low Vision Devices
The patient reported being very happy with the outcome over the previous months. The low vision devices greatly increased her quality of life, citing that she was doing things she had not considered she would be able to do, such as reading small prescription details on medication bottles. No change to her current lens hygiene, wearing schedule, prescription, or low vision device use was recommended.
Discussion/Alternative Management Options
This patient presented to the clinic as a long time, thirty plus year wearer of GP corneal lenses. She had specific complaints about comfort of the lenses in dusty environments and mentioned difficulty being able to read fine print on medication bottles at her job as a traveling nurse in developing nations. A refraction was performed to determine her best corrected visual acuity in spectacles. A corneal topography and a thorough slit lamp examination were utilized to assess the state of her condition, specifically to evaluate the shape of the cornea in consideration of different contact lens modalities and treatment options. Given the reduced best corrected visual acuity in spectacles and the information gained from the corneal topography and slit lamp examination, several treatment options were weighed and contrasted.
The first consideration was to refit her GP lenses; however, the patient had a specific complaint about the comfort of the lenses with dust and debris during lens wear. One well known drawback to corneal GP lenses is the increased likelihood for debris to get under the lens.10 Fitting of corneal GP lenses relies on the principal of the central zone just clearing or aligning with the central cornea, and the mid-periphery of the lens fitting uniformly with the curvature of the ocular surface.10 The patient’s topography and slit lamp examination were significant for a highly irregular anterior corneal surface, secondary to the hyaline deposits displacing her corneal epithelium in the areas where a small diameter lens would come into contact with the ocular surface, complicating her fit. Larger diameter, intralimbal, corneal lenses were also considered to vault the irregularity, but they would not address the concern for discomfort in dusty environments.
Scleral lenses offer several advantages over traditional GPs. For this case in particular, the irregularity of the post-surgical ocular surface and anterior hyaline deposits would be vaulted entirely by the lens. The saline filled tear layer corrected the irregular astigmatism induced by deposits and isolated the reduction in visual acuity as a result of the granular opacities alone. Visual acuity with an over-refraction in scleral lenses increased acuity by two lines. Scleral lenses are also not as susceptible to debris getting under the lenses in dusty environments and are generally reported as more comfortable than corneal lenses. The patient was very receptive to scleral lens wear as a treatment option.
Other options considered were soft contacts lenses and hybrid soft contact lenses. The patient was very vocal about her prior attempts in the 1990s to wear soft contact lenses and how uncomfortable they were for her. She did have mild dry eye as noted with her tear break up time of five seconds in each eye. Soft contact lens wear may be contraindicated in patients suffering from dry eye and patients may report higher levels of dryness with soft contact lens wear. This patient also travels to austere environments where storage and hygiene considerations may present a higher risk for microbial keratitis with soft contact lens wear versus GP lenses. Soft contact lenses would do nothing to address the irregularity created by the hyaline deposits. She stated that she was not interested in any sort of soft lenses.
Further surgical options were discussed with the patient. The patient had previously undergone two separate keratectomy procedures and was told she would not be eligible for a third by her corneal surgeon. If her condition progressed to where spectacles and contact lenses could no longer correct her vision to allow her to perform her activities of daily living, her next option would be a full thickness corneal transplant. The patient’s father had a corneal transplant with a poor outcome earlier in the patient’s lifetime and she was viscerally opposed to the consideration of a transplant, stating she would rather stop working and retire. The patient was open to two options, refitting her current GP modality or scleral contact lenses. The scleral lenses offered improved comfort, less likelihood of debris getting under the lenses, and improved visual acuity, so scleral lenses were selected as the best modality to meet the patient’s goals for vision and comfort.
In this case report, a combination of scleral lenses and low vision devices were utilized to improve reduced visual acuity in a patient with Granular Corneal Dystrophy Type I. The dual approach was indicated due to two etiologies for reduced visual acuity: irregular corneal ocular surface status-post bilateral, superficial keratectomy and opacification secondary to the stromal dystrophy. This case illustrates a multifaceted approach to meet the visual demands of a complicated case presentation. The patient has been utilizing scleral lenses for more than a year and is extremely satisfied with the comfort and vision in the lenses. She has been very pleased with the addition of the low vision devices. The combination approach has allowed her to continue to work with independence as a nurse and have increased her capacity to enjoy her leisure activities outside of work.
References
- Ehlers, JP, Shah, CP. The Wills Eye Manual. Office and Emergency Room Diagnosis and Treatment of Eye Disease. Fifth Edition. 2008 Lippincott, Williams & Wilkins. Philadelphia. 91-93.
- Kanski, JJ, Bowling, B. Clinical Ophthalmology, A Systemic Approach. Seventh Edition. Chapter 6: Cornea: Keratoconus. 2011. Elsevier London. 210-211
- Kwan, J, Dalton, K, Weissman, B. Contact Lens Applications and Corneal Dystrophies: A Review. Eye and Contact Lens: Science and Clinical Practice. 2016;42 (3):177-184.
- Kazutaka, K, Hidenaga, K, Akihito, I, Nobuyuki, S, Kimiya, S. Effect of Light Scatterign and Higher-order Abberrations on Visual Performance in Eyes with Granular Corneal Dystrophy. Scientific Reports. 2016;6:24677.
- Taneja, M, Rathi, V, Murthy, S, Bagga, B, Vaddavalli, P. Femtosecond Laser-Assisted Anterior Lamellar Keratoplasty for Recurrence of Granular Corneal Dystrophy in Postkeratoplasty eyes. Cornea: The Journal of Cornea and External Disease 2017;36 (3): 300-303.
- Steger, b, Romano, V, Biddolph, S, Willoughby, C, Batterbury, M, Kaye, S. Femtosecond- Laser Assisted Lamellar Keratectomy for Corneal Opacities Secondary to Anterior Corneal Dystrophies: An Interventional Case Series. Cornea: The Journal of Cornea and External Disease 2016;35 (1):6-13.
- Barnett, M, Lein, V, Li, J, Durbin-Johnson, B, Mannis, M. Use of Scleral Lenses and Miniscleral Lenses After Penetrating Keratoplasy. Eye and Contact Lens: Science and Clinical Practice 2016;42 (3):185-189.
- Lee, J, Chiu, G, Bach, D, Bababeygy, S, Irvine, J, Heur, M. Functional and Visual Improvement With Prosthetic Replacement of the Ocular Surface Ecosystem Scleral Lenses for Irregular Corneas. Cornea: The Journal of Cornea and External Disease 2013;32 (12):1540-1543.
- Valley Contax, Custom Stable Elite, Custom Stable fitting guide. Accessed online 20 July 2017. http://www.valleycontax.com/files/custom-stable-fitting-guide.pdf
- Gasson, A, Judith, M. The Contact Lens Manual. A Practical Guide to Fitting. Fourth Edition. Edinburgh, London, England. 2010:126-146.
- DeNaeyer, G, Sanders, D, van der Worp, E, Jedlicka, J, Michaud, L, Morrison, S. Qualitative Assessment of Scleral Shape Patterns Using New Wide Field Ocular Surface Elevation Topographer. Journal of Contact Lens Research & Science. 2017;1(1):16.
Back to Table of Contents
