Innovative Lens Customizations for a Keratoconus Patient After Corneal Crosslinking Treatment: Clark Chang, OD, MSA, MSc, FAAO
Background
A 19-year-old white male patient, VD, started complaining of night halo and glare about 12 months ago, worse in spectacles than his soft toric disposable lenses. As per VD, his frequent spectacle prescription changes in the past were deemed normal due to his young age; otherwise, there was no clinical reason or diagnosis given for his chief complaints from previous eye exams. As well, his medical history and family history were non-contributory. Below is a brief summary for his baseline examination.
| OD | OS | |
| VA (with Habitual Soft CL) | 20/25-2 | 20/25 |
| Habitual Soft CL Rx | 8.5/-4.75, -0.75 x090 | 8.5/-3.50, -1.50 x065 |
| MR (Manifest Refraction) | -4.00, -1.75 x110 | -2.75, -2.25 x095 |
| MRVA | 20/20-1 | 20/20-3 |
| Keratometry | 45.75/44.50 x085 | 44.50/44.00 x105 |
| Pachymetry (Ultrasound) | 533 | 549 |
| Slit Lamp findings (Anterior Segment/Posterior Segment) | All findings are within normal limits | All findings are within normal limits |
Corneal elevation data from tomographic studies supported a diagnosis of keratoconus (KC) suspect, OU (Fig. 1A & 1B). Patient was educated about both the likely diagnosis of early KC and corresponding treatment options such as corneal cross-linking (CXL) to halt the progression and post-operative uses of specialty lenses to improve quality of vision. Patient was further educated about CXL procedure costs and potential insurance coverage for the US Food and Drug Administration (FDA) approved epithelium-off CXL protocol. As the patient agreed to short-term monitoring in hopes of possible insurance coverage, VD was asked to return to clinic in four months, or sooner if he experiences further decreases in vision.
VD return to clinic in four months and tomography studies revealed mild KC progression, OD greater than OS (Figure 2). The patient continued to complain of night halo and glare, but he was uncertain if visual acuities had changed in OD and OS. As a result of this examination, VD was referred for CXL consultation at a local cornea clinic. Again, the patient was educated on contact lens refitting to help rehabilitate his vision after CXL. Patient was advised to return to clinic to discuss contact lens treatment options at three months post-CXL, unless the co-managing corneal specialist instructed the patient of a different timeframe due to individualized recovery course post-CXL.

Contact Lens Evaluation #1
VC returns to clinic for contact lens evaluation at three months after uncomplicated CXL procedures. While mild CXL haze can be appreciated during the slit lamp examination, it was deemed non-visually significant and expected to continue to resolve on its own (Figure 3).

As VD exhibited the expected corneal findings during a typical post-CXL recovery course, keratoconus contact lens options were discussed with him. Hybrid lenses were recommended as they can offer the visual benefits of a corneal gas permeable (GP) lens and still retain some familiarity to soft lens platforms to which that VD had successfully adapted. However, VD was educated about the potential of improved but persistent night glare given his mesopic pupils measured at 8mm OU, which is larger than the general designated optical zones in hybrid lens designs. However, given many keratoconus patients report great improvements in visual functions with small diameter corneal GPs and a hybrid lens design with larger optical zone would be utilized, it was deemed a good initial treatment choice for VD.
| OD | OS | |
| Diagnostic Lens (Hybrid CL) | SynergEyes A/7.2/8.2/-6.00 | SynergEyes A/7.3/8.3/-5.00 |
| Spherical OR (Over-CL Refraction) | -0.75 | Plano |
| VA (with Spherical OR) | 20/20-1 | 20/20-3 |
| Sphero-Cylindrical OR | -0.50, -0.50 x090 | Plano, -0.50 x100 |
| VA (with Sphero-Cylindrical OR) | 20/20+2 | 20/20+2 |
| Keratometry (Taken Over Hybrid CL) | 41.75/41.00 x085 | 41.75/41.00 x130 |
| Slit Lamp Exam | ||
| Lens Vault | Good clearance under Center-GP & at Junction | Good clearance under Center-GP & at Junction |
| Lens Position & Movement | Centers & Good movement | Centers & Good movement |
| Final Lens Parameters | 7.2/8.2/-6.50/EP | A/7.3/8.3/-5.00/EP |
During diagnostic fitting process, VD subjectively reported much more significant improvement in visual symptoms with a sphero-cylindrical over-refraction, when compared to a spherical over-refraction. As this is a possible optical effect of lens flexure, incorporation of thickened lens profiles and/or inclusion of front surface toricity have in some cases proven to be useful as counter measures. Given that the patient is eager to return to best visual performance as quickly as possible and this particular hybrid lens design has only the option of a thicker center, it was decided to customize VD’s lens design, OU, with the enhanced profile (EP) feature. VD was also educated on uses of a hydrogen peroxide lens care solution for daily disinfection and preservative-free saline solution for lens application. In the case that patient experiences night halo and glare with hybrid lenses, VD was given a prescription of Brimonidine Tartate 0.1% ophthalmic solution to use on eyes without hybrid lenses. The patient instructed to wait 15 minutes prior to re-applying hybrid lenses before going out at night time. Also, VD was asked to return to the clinic at 4 to 6 weeks after lens dispensing.

Contact Lens Evaluation #2
Patient reported good comfort with hybrid lenses with full day wear. Although his overall vision has improved, he had only experienced a slight reduction in his symptoms of night visual disturbances. In addition, installation of Brimonidine Tartate 0.1% ophthalmic solution does appear to further help with some level of reduction in such halo and glare symptoms. Moreover, despite no serious issue with lens insertion, the patient inquired if there are specialty lens options that do not require application solution during lens insertion process.
| OD | OS | |
| VA (with Hybrid CL) | 20/20 | 20/20 |
| Spherical OR (Over-CL Refraction) | Plano | Plano |
| VA (with Spherical OR) | 20/20 | 20/20 |
| Sphero-Cylindrical OR | No Improvement | No Improvement |
| Slit Lamp Examination | ||
| Lens Vault | Good clearance under Center-GP & at Junction | Good clearance under Center-GP & at Junction |
| Lens Position & Movement | Centers & Good movement | Centers & Good movement |
| Cornea, Bulbar/Palpebral Conjunctiva | All findings are within normal limits | All findings are within normal limits |
Due to improved night vision with Brimonidine Tartate 0.1% ophthalmic solution, it appeared that large mesopic pupils exacerbates VD’s visual symptoms of night flare in addition to irregular corneal optics. Therefore, VD was offered to be fit in an intra-limbal GP lens design with a fitting approach to accommodate for a larger optical zone. Given the possibility of decreased initial comfort with a corneal GP, the patient was educated about the need for longer adaptation time at the beginning after first receiving corneal GPs. Due to slit lamp observation of mild inferior GP decentration and mild apical touch, OU, it was decided to mildly steepen base curve from the diagnostic GP used in-office. As well, lens diameters were increased in both eyes to accommodate the larger optical zone (OZ) needed. VD was educated to continue to use hydrogen peroxide lens care solution for GP lens disinfection, but preservative-free saline is not absolutely required during lens insertion.
| OD | OS | |
| Diagnostic Lens (Corneal GP CL) | 7.76/11.0mm/-3.00 | 7.76/11.0 mm/-3.00 |
| Spherical OR (Over-CL Refraction) | -0.25 | +0.50 |
| VA (with Spherical OR) | 20/20 | 20/20 |
| Slit Lamp Examination | ||
| Lens Vault | Mild apical touch & good edge lift clearance | Mild apical touch & good edge lift clearance |
| Lens Position & Movement | Mild inferior decentration & Good GP movement | Mild inferior decentration & Good GP movement |
| Final Lens Parameters | 7.67mm/-3.75/11.2mm/ Larger OZ of 10.0mm/PC 1 Step Steep | 7.71mm/-2.75/11.2mm/ Larger OZ at 10mm/PC 1 Step Steep |
Contact Lens Evaluation #3
VD returned to the clinic after four weeks of adaptation time with corneal GPs. Patient reported good lens tolerance, improved vision, and reduced night visual disturbances. He does not think installation of Brimonidine Tartate 0.1% ophthalmic solution helps to deliver further improvement in quality of vision, so he has not trialed usage of Brimonidine Tartrate 0.1% since switching to GP lenses. However, the patient still felt insecure with his mobility and driving activities at night; as such, he is considering dropping out of college as he is unable to attend his evening classes and unable to withstand the bright sunlight when sitting in classroom during day time. In fact, he has recently started therapy with a psychologist because he feels depressed about not being able to continue his studies and his activities of daily living.
| OD | OS | |
| VA (with GP lenses) | 20/20 | 20/20 |
| Spherical OR (Over-CL Refraction) | Plano | Plano |
| VA (with Spherical OR) | 20/20 | 20/20 |
| Sphero-Cylindrical OR | No Improvement | No Improvement |
| Slit Lamp Examination | ||
| GP-Cornea Fitting Relationship | Mild apical clearance & Good edge lift | Mild apical clearance & Good edge lift |
| Lens Position & Movement | Good GP position & Movement | Good GP position & Movement |
| Cornea, Bulbar/Palpebral Conjunctiva | All findings are within normal limits | All findings are within normal limits |

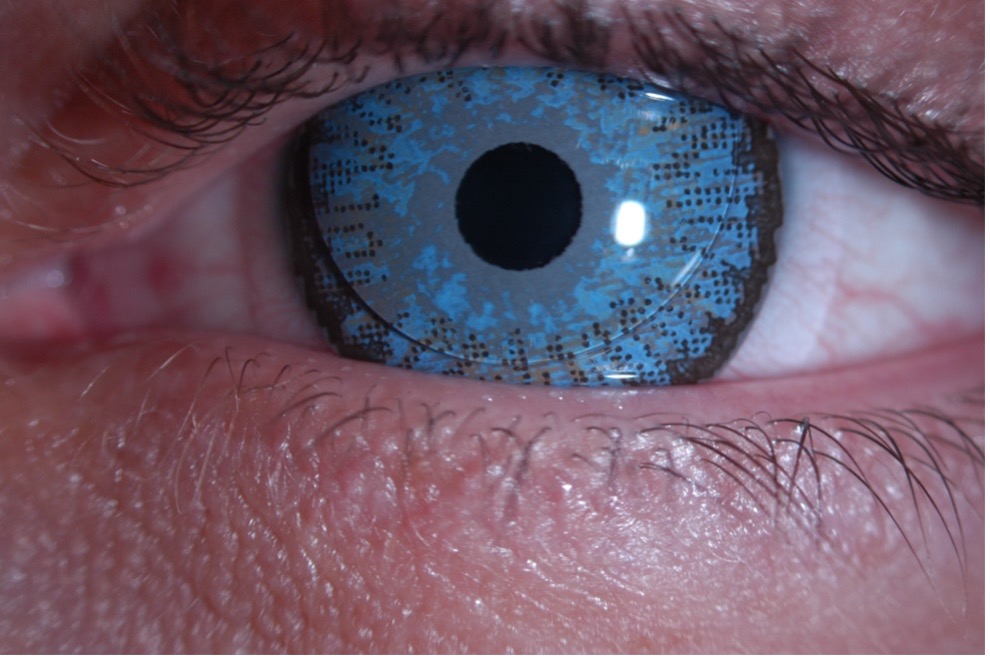
VD was educated on potential use of a soft color prosthetic lens with a small painted pupil in a piggyback system with his current GP to maximize the negative impacts of his visual symptoms. The patient was educated on more limited oxygen permeation through a painted soft hydrogel lens and the need for long-term monitoring as well as good patient compliance with wearing instructions. In this case, a blue iris print was selected to match the patient’s original eye color with a black underprint and a 3.0mm clear pupil. Prior to ordering soft color prosthetic lenses, a piggyback fitting relationship was simulated in clinic. Clear soft disposable trial lenses that were available in the office were used to determine the suitability of current corneal GP lenses in their utilization within a piggyback system as well as to demonstrate wearing experiences of piggyback lenses to VD.
| OD | OS | |
| Final Lens Parameters | Durasoft 3 Colorblend Blue/8.3/Plano/3.0mm open pupil/Black underprint | Durasoft 3 Colorblend Blue/8.3/Plano/3.0mm open pupil/Black underprint |
Contact Lens Evaluation #4
VD returned to the clinic reporting significant reduction in photophobia, halos, and glare. While he occasionally experienced a small amount of halos and glare at night, he could resume his school activities and daily living activities. The patient not only reported good vision and comfort, he also found lens handling and care to be easy since he did not have to fill up his lenses with preservative-free saline solution during lens application. VD continues to use hydrogen peroxide contact lens solution to perform daily disinfection of his piggyback lens system. He was educated on replacement frequencies of each lens design as well as the need for ongoing cornea monitoring.
| OD | OS | |
| VA (with Piggyback CL) | 20/20 | 20/20 |
| Spherical OR (Over-CL Refraction) | Plano | Plano |
| VA (with Spherical OR) | 20/20 | 20/20 |
| Slit Lamp Examination | ||
| Piggyback-Cornea Fitting Relationships | Mild GP clearance over soft CL & Acceptable edge lift | Mild GP clearance over soft CL & Acceptable edge lift |
| Lens Position & Movements | GP & SCL both center and exhibit good movement | GP & SCL both center and exhibit good movement |
| Cornea, Bulbar/Palpebral Conjunctiva | All findings are within normal limits | All findings are within normal limits |
Discussion
The negative psychological impacts of keratoconus to one’s quality of life should not be underestimated. Moreover, clinical evidence also reveals that cumulative effects of such ocular conditions further deteriorate over one’s life span1,2. This case demonstrates the importance of early keratoconus detection in maximally preserving a patient’s visual function throughout his or her lifetime. Nonetheless, the majority of keratoconus patients will experience most visual improvement with contact lenses. Therefore, contact lens treatment options should no longer to viewed as strictly a pre-surgical treatment option; rather, contact lenses can also compliment the beneficial effects of medical and surgical treatment by rehabilitating patients’ visual performances after such medical and/or surgical interventions.
Because every person living with keratoconus have different needs, it is essential to look at the entire patient profile, and not just focusing solely on ocular characteristics, when deciding on contact lens treatment options. It is important to recognize that all lens designs have their own unique advantages and challenges; thus, doctors and patients are encouraged to consider all lens options thoroughly and keep an open mind about the wide array of lens options available. In the case of VD, the unique use of a color prosthetic soft lens in a piggyback system allowed this young patient to continue pursuing his education and training. And he continues to return to clinic for his cornea monitoring every six months with no complications to date.
References
- Kymes SM, Walline JJ, Zadnik K, Gordon MO; Collaborative Longitudinal Evaluation of Keratoconus study group. Quality of life in keratoconus. Am J Ophthalmol. 2004 Oct;138(4):527-35.
- Kymes SM, Walline JJ, Zadnik K, Sterling J, Gordon MO, Collaborative Longitudinal Evaluation of Keratoconus Study Group. Changes in the quality-of-life of people with keratoconus. Am J Ophthalmol. 2008;145(4):611-617.
Back to Table of Contents


