Advanced Presbyopia: Segmented, Translating Bifocal: Robert L. Davis, OD, FAAO
Background
JM was a 68 year old female flower shop owner interested in improved vision from her soft lens bifocal lenses. She has worn rigid lenses in the past for over thirty years and was refitted by another practitioner because of what she described as blisters on the corner of her eyes. JM also explained that later in the day her eyes became sensitive to the light and felt sandy and irritated. She has been taking glaucoma medications for five years because of elevated intraocular pressure.
JM was interested in returning to rigid lenses because the soft lenses lacked the crispness of vision and they were more difficult to handle than gas permeable lenses. JM’s goals in wearing gas permeable rigid lenses is to provide clear and consistent vision at all working ranges without the need of using store-bought reading glasses for small detail at near. JM also wanted to increase wearing contact lenses at night without feeling irritated.
Medications include celebrex, norvasc, ecotrin, hisinopril, toprol, crestor, furesemide, furesemide folgard and betagan.
Previous contact lens specifications:
| OD | OS | |
| Base Curve Radius: | 8.7mm | 8.7mm |
| Overall Diameter | 14.4mm | 14.4mm |
| Back Vertex Power: | -1.00/+2.00 D lens | -1.00/+2.00 D lens |
| Material: | Omifilcon | Omifilcon |
Manifest Refraction:
OD: -1.00 – 1.00 x 010 Add: +2.25D
OS: -0.75 – 0.50 x 170 Add: +2.25D
Keratometry (sim K’s)
OD 43.25/44.25
OS 43.00/44.00
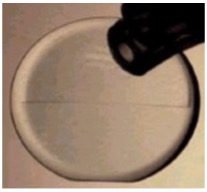
(See Figure)

Intraocular Pressure:
OD: 24mmHg
OS: 25mmHg
Pachymetry:
OD: 540
OS: 560
Dry Eye evaluation:
OD: Low tear meniscus without debris was present. Tear Break-Up-Time (BUT) was 6 seconds. Superficial punctate staining was also present.
OS: Low tear meniscus without debris was present. Tear BUT was 8 seconds. Superficial punctate staining was also present.
Pupil size: 3.8mm (mesopic); 4.5mm (scotopic)
Slit Lamp Evaluation: Upper lid eversion exhibited normal palpebral conjunctiva without hyperemia. Lower lid on line of pupil O.U. Grade 1 nuclear sclerosis was present OU. Grade 1 bulbar hyperemia O.U. and Grade 1 anterior blepharitis were present. The punctum exhibited a .6mm opening. All other biomicroscopy findings were normal.

JM’s tear film layer instability is inadequate to support contact lenses. Glaucoma therapy can become toxic to the corneal epithelium with the increase use of benzalkonium chloride(BAK) preserved solutions added to the ocular tear film. Selective use of glaucoma therapy needs to be controlled to limit the use of toxic agents placed onto the ocular surface. Along with the change of medication, increased contact time will also help the medication reach a therapeutic effect. JM was explained the possible causes of her dry eye and the remediation of both the dry condition and glaucoma therapy. JM was also explained that due to her large opening to the tear drainage system, plugging one of the drains in each eye will reduce the tear film draining into her nose. In addition this will deliver additional medication to the ocular surface by increasing therapeutic contact time. Punctal occlusion was suggested and a change of her glaucoma medication to Travatan Z to eliminate BAK use and to reduce the instillation of the medication to once per day before bedtime. Heat and eyelid scrubs were also suggested to improve the tear film and eliminate the blepharitis.
JM was instructed to wear her glasses for the next two weeks until the ocular surface improved to support contact lens wear. I assumed that her previous gas permeable contact lens experience failed because of 3 & 9 o’clock staining caused by the dry eye condition. Soft lenses immediately improved the contact lens subjective experience because of the bandage effect of the soft lens in the short term. Without solving the underlying dry eye and blepharitis problem, contact lens failure would be experienced again.
JM was immediately placed on Travatan Z before bedtime, heat and lid scrubs twice a day, Soothe eye drops in the morning and at night, and punctal occlusion. A follow-up visit was scheduled for two weeks.
At the follow-up visit the blepharitis had cleared up completely, the tear meniscus was at a normal level and the Tear BUT was 18 seconds for OD and 19 seconds for OS. Her symptoms of photophobia had been eliminated and the eyes felt normal. The intraocular pressure was 18mmHg OD and 17mmHg OS. No corneal staining was exhibited after fluorescein instillation.
The Fitting Process
JM was told that we can proceed with the contact lens fitting and that we would attempt to meet all of her visual expectations. The average keratometry values were used as the starting point of the fitting process. Lenses were viewed through the slit lamp and experienced good movement and translation. Fluorescein was instilled and good alignment was experienced with peripheral pooling. The inferior flat portion of the lens rested upon the lower lid. Due to the curvature of the lower lid the lenses positioned slightly temporal OU. If consistent temporal placement was exhibited, the prism placement would be compensated for aligned optics. The pneumonic “Right-Add, Left-Subtract” (RALS) is used to either add if the rotation is to the practitioners right or subtract if the rotation is to the practitioners left.
Lens parameters Tangent Streak Bifocal
| Base Curve Radius | Overall/Optical Zone Diameter | Power | Material | Seg Height | Prism | |
| OD | 7.95mm | 9.4/9.0mm | -0.50/+2.00D Add | SGPII Blue | 4.2 | 2@90 |
| OS | 7.95mm | 9.4/9.0mm | -0.25/+2.00D Add | SGPII Blue | 4.2 | 2@90 |
Dispensing Visit
Lenses were placed in the eye after topical anesthetic application to effectively evaluate the fit without tearing and to optimize the comfort for a positive contact lens experience.
Visual Acuity (Distance and Near)
OD: 20/20 (Distance); 20/20 (Near)
OS: 20/20 (Distance); 20/20 (Near)
Slit Lamp Evaluation: The lenses were supported by a good tear film with the truncation of each lens adjacent to the lower lid.
A patient education program was instituted to establish good hygiene and cleaning/ disinfection routines. The Boston Conditioning Solution and Boston Cleaner (Bausch + Lomb) care regimen was explained to the patient. The patient was also instructed how to use the bifocal lens design by moving the reading card from a straight position to moving the card inferiorly until reading was experienced and then again moving the card superior until the reading card was blurred. This illustrated to the patient where the bifocal line was placed in the field of view as well as giving me an idea if the line of seg was properly positioned. The wearing time was initially started at six hours and increased two hours each day until eight hours was achieved. After eight hours was achieved, the patient was instructed to wear the lens design all her waking hours. A follow-up visit was scheduled for one week.
Follow-Up Care/Final Outcome
JM was evaluated eight days after dispensing and described her vision as it was many years ago. Both distance and near were pristine and the movement from distance to near and back to distance was seamless. Post-fit corneal topography showed the effects of the lens on the eye after fourteen hours of wear. The left lens exhibited slight apical clearance although corneal integrity at the 3 & 9 o’clock position remained intact. Careful observation of this area over time might ultimately result in the need for a slightly flatter base curve radius. The photophobia was eliminated and she could wear her lenses 12 to 14 hours without them feeling tired. She also liked instilling the glaucoma medications before bedtime and asked if she should still use the Soothe eye drops. I explained that the eye drops would help maintain her oily layer of the tear film which helps reduce evaporation. Punctal plugs helped to reduce her pressure and, more importantly, increased the tear volume remaining in the eye instead of draining into the nose. This would maintain the tear volume that is necessary to support the contact lens moving on the eye. Without the tear volume the lens would ride on the surface of the eye creating the blister she experienced before. No conjunctival hyperemia was experienced during the wearing time and no staining was exhibit upon fluorescein instillation.
Discussion/Alternative Management Options
This case demonstrates the need to solve medical effects upon the ocular surface to support contact lens wear. The total clinical observation needs to be examined to discover the problems associated with contact lens wear. Other lens modalities could have been selected although listening to the patients expectation lead to the selection of the alternating lens design. The patient is your partner in selecting the appropriate contact lens therapy. Understanding the patient’s goals and the difficulties presented in achieving these goals clearly represents our therapeutic approach.
Back to Table of Contents
