Corneal Neovascularization: John M. Rinehart, OD, FAAO
Background
38 year old male presented wearing low Dk, non silicone-hydrogel toric soft contact lenses. His current lenses are three years old and he has recently lost his left lens. He is very pleased with his current prescription. He has not worn lenses for three weeks and he has no spectacles.
Test Procedures/Fitting & Refitting Lens Designs & Ordering
Unaided Visual Acuity (Distance):
OD 20/250
OS 20/200
Manifest Refraction:
OD -7.00 -0.50 x 100 20/20
OS -4.50 -2.25 x 180 20/20
Keratometry:
OD 46.00 @ 180; 47.00 @ 090 mires clear
OS 44.75 @ 180; 46.75 @ 090 mires clear
Biomicroscopy:
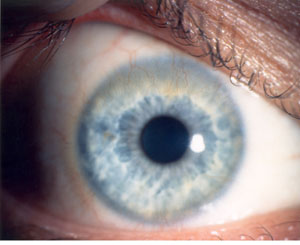
Grade 3 neovascularization (see photo) is present in the right eye. The left eye exhibits Grade 2 neovascularization, primarily ghost vessels.
The patient was fit with corneal gas permeable (GP) contact lenses in order to increase the amount of oxygen available to the cornea and to minimize any physical irritation of the limbal vessels.
To achieve an apical alignment fit it was necessary to fit the right lens somewhat flatter than “K”. The final base curve radius was: OD 0.75 D flatter than flat “K”; OS “on flat K”.
Patient Consultation and Education
Considerable time was devoted to discussing the risks to vision by allowing the blood vessels to continue to grow further into the cornea. The importance of timely examinations and monitoring was emphasized as neovascularization causes no discomfort and is not something the patient can monitor himself.
Follow-Up Care/Final Outcome
The lenses were dispensed and the patient was instructed in application, removal and care of the lenses. He began by wearing the lenses five hours the first day and increased two hours per day after that. Appointments were scheduled one and three weeks after lens dispensing. By the three-week appointment all the blood vessels in the cornea were empty. The patient was scheduled to be followed again in four months in order to monitor the blood vessels.
Discussion/Alternative Management Options
The options discussed with this patient were to be fit with silicone-hydrogel toric soft contact lenses, fit with corneal gas permeable lenses, or prescribed spectacles. Given the patient’s refractive error and the thickness profile of his soft contact lenses, reducing contact lens wearing would also be indicated. If a daily disposable option is prescribed, silicone-hydrogel material would be recommended. Higher oxygen permeability and reduced wearing time is highly recommended to reduce hypoxia and continued growth of the blood vessels.
Several factors that may cause neovascularization including hypoxia, mechanical stimulation, allergies, and infections.(1) Today’s high Dk GP and high-Dk silicone-hydrogel materials minimize the risk of hypoxia. GP lenses and silicone-hydrogel lenses with higher modulus can occasionally contribute to neovascularization.(2)
Fonn et al.(3) reported that ~65% of patients wearing low-Dk non-silicone soft lenses on an extended wear basis exhibited corneal neovascularization. Whereas, no patients showed neovascularization in a study of patients wearing silicone hydrogels on an overnight wearing schedule. Also, corneas that exhibited neovascularization after low-Dk non-silicone lens wear showed regression with ghost vessels replacing the neovascularization.
Suggested Readings
1) Campbell JB, Henry VA, Woo S. Soft lens problem solving. In Bennett ES, Henry VA. Clinical Manual of Contact Lenses. 4th Ed. Philadelphia, Lippincott Wolters & Kluwer, 2014:313-341
2) Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Anterior Eye 2002;25:137-146
3) Fonn D, MacDonald KE, Richter D, et al. The ocular response to extended wear of a high Dk silicone hydrogel contact lens. Clin Exp Optom 2002;85:176-182
Back to Table of Contents
